September 1, 1995
Air Date: September 1, 1995
SEGMENTS
Antibiotic Resistance
/ Bob CartyFaced with a barrage of medicinal attack, bacteria are fighting back. The strongest are adapting and surviving the onslaught of antibiotics which most doctors eagerly dispense, and their patients demand. Should the medical community curb widespread use of antibiotics? Do patients compromise their immune systems by going for a fast fix? Bob Carty of the Canadian Broadcasting Corporation reports. (14:34)
Evolutionary Medicine: Rethinking the Origins of Disease
Author Marc Lappé suggests an approach to healing which relies less on chemical drugs and more on the body's natural defenses. He's convinced that the human impact on the natural world is at the root of many new strains of infectious diseases which are filling our hospitals, including AIDS and tuberculosis. This program originally aired in March, 1995. (06:07)
Show Credits and Funders
Show Transcript
Copyright (c) 1995 by World Media Foundation. No portion of this transcript may be copied, sold, or transmitted without the written authority of World Media Foundation.
HOST: Steve Curwood
NEWSCASTER: Jan Nunley
REPORTERS: Jennifer Schmidt, Bob Carty
GUEST: Marc Lappé
(Theme music intro)
CURWOOD: From National Public Radio, this is Living on Earth.
(Music up and under)
CURWOOD: I'm Steve Curwood.
We thought we had them licked, but old diseases are coming back stronger than ever and resistant to drugs. Why? Doctors say we've changed the ecology of the bacterial world with the heavy use of antibiotics.
LAPPÉ: We've essentially created our own nightmare by neglecting the value of vaccines, immunization, and natural controls, and instead of relying entirely on this myth that a chemotherapeutic approach is an impenetrable barrier.
LEVY: It's hard to make a comparison with other forms of ecologic change, such as burning of the rainforest, but I must say antibiotics are doing a similar thing.
CURWOOD: Coming up this week on Living on Earth, right after this news.
Environmental News
NUNLEY: From Living on Earth, I'm Jan Nunley. Lead-free water faucets will now be available to consumers nationwide as part of a landmark agreement between environmental groups and manufacturers. The settlement ends a lawsuit filed in 1992 by the Natural Resources Defense Council and the Environmental Law Foundation. More than a dozen manufacturers were accused of selling faucets that leach lead into drinking water. Seven of the companies Including American Standard, Masco , and Whirlpool have agreed to remove lead from 95 percent of their products in the next five years. A spokesman for Masco, maker of Delta and Peerless faucets. says the company feels exonerated because the settlement requires other companies to do what they have been doing voluntarily for years.
Environmental activists hope the North American Free Trade Agreement can bring a halt to salvage logging in the northwest. They've filed a formal complaint charging the U.S. with failing to enforce its environmental laws as required by NAFTA. From Seattle, Jennifer Schmidt of KPLU reports.
SCHMIDT: The complaint was filed on behalf of more than 2 dozen environmental groups. It targets the new U.S. timber salvage program which exempts logging of diseased and fire damaged trees from environmental law. Sierra Club Legal Defense Fund attorney Patty Goldman says by restricting court challenges, the salvage program violates core provisions of NAFTA.
GOLDMAN: The NAFTA environmental side agreement has two overriding principles throughout. One is that a country must have effective enforcement and the other is that the public must have a way to ensure that there's enforcement by seeking investigations, by being able to introduce information with respect to a governmental decision, and to be able to challenge that decision, the final decision.
SCHMIDT: The complaint was filed with a NAFTA environmental commission in Montreal. The commission is already pursuing two other cases. The commission cannot strike down the salvage law, but it can pursue an investigation, and if it finds a violation has occured, Canada and Mexico could demand trade sanctions. For Living On Earth, I'm Jennifer Schmidt in Seattle.
NUNLEY: One species of sea turtle may be making a comeback. Researchers in Florida have counted more Loggerhead sea turtle nests along Broward County beaches this year than ever before. The Loggerhead is listed as a threatened species and nearly 40 percent of all the turtle's nests are in Florida. Researchers are leery of making predictions based on a single year since Loggerhead turtles lay eggs many times in one season and then don't nest again for several years. The current peak could be followed by a large drop. But Dr. Peter Pritchard of the Florida Audubon Society says there's been an irregular but progressive increase in their numbers since 1973, when people were banned from taking the turtle's eggs.
Efforts are underway to return Grizzly bears to an area near the Bitterroot Mountains of Montana and Idaho and nearly two-thirds of the people polled in those states favor reintroducing the animals as a way of preserving them from extinction. Officials say the show of popular support for the grizzlies is particularly encouraging because of earlier legal battles over reintroducing wolves into those states. Ranchers fought for a decade to stop the restoration of wolves to the area.
Under new G.O.P budget proposals, government funding for environmental research would be cut by nearly 20 percent by the year 2002. The American Association for the Advancement of Science says those cuts would mean scrapping research and development for the E.P.A, the Interior Department . . and the U.S. Forest Service. Overall R&D funds would be cut nearly 33 percent, a decrease of more than 5-and-a-half billion dollars. While the association warns of the impact of these cuts on the future of American science, many conservatives say federal subsidies for research are unnecessary. Jerry Taylor is Director of Natural Resource Studies for the Cato Institute in Washington, D.C.
TAYLOR:The fact is, is that yes we like new technology, yes we like Research and Development, but by-and-large those sorts of things happen in a free economy without government subsidy.
NUNLEY: The current Congress has already cut funds for most non-defense research by more than 5 percent.
There's nothing wrong with taking your work home with you, but an official at Japan's Institute for Cetacean Research apparently took it too far when he served whale for dinner. Reuters reports that Kazuo Yamamura asked a research vessel hunting Minke whales to set aside some slices of harpooned whale for him. The meat was later served as sashimi at a party Yamamura gave at the Tokyo University of Fisheries. Yamamura told Reuters his motive for serving up his own research was that he "wanted to give normal people a chance to eat whale meat."
Officially, Japan does hunt whales for population studies. But environmentalists say most of the meat - an expensive delicacy - ends up in restaurants, and not laboratories. Commercial whaling has been banned worldwide since 1985 by the International Whaling Commission. Most countries want a ban on Japanese-style research whaling as well.
That's this week's Living on Earth news. I'm Jan Nunley.
(Theme music up and under)
Antibiotic Resistance
CURWOOD: This is Living on Earth. I'm Steve Curwood. Something is going terribly wrong with our antibiotics. These drugs have saved millions of lives in the 20th century, but they are suddenly not curing certain diseases any more. In fact, in the US, 70% of all infections that people get while in the hospital are now resistant to antibiotics. The reason, many scientists say, is simple ecology. Bacteria and the other microorganisms live in balance with each other and humans. Antibiotics upset that natural balance by killing off the most susceptible germs. But those which survive are the strongest and most deadly. And these germs can multiply with astonishing speed, since they figured out how to beat antibiotics, and they no longer have to compete with their more benign cousins. Bob Carty has our report.
THEROUX: My name is Camille Theroux, and I was a truck driver. I went in on the 22nd November '92 for an aneurism operation.
DOCTOR: Complications ensued, which required application of many antibiotics aimed at preventing him from getting more ill.
THEROUX: 13 different types of antibiotics.
DOCTOR: The result of all this was in due course that he developed totally antibiotic-resistant organisms.
THEROUX: Where this came from I have no idea, this bacteria eating me out, you know. And I still don't know what it is.
(Hospital monitors beep; hospital workers talk)
CARTY: His friends call him Tiny, and he's a living bookmark in medical history. While in an Edmonton hospital, Tiny developed an infection his doctors had never seen before. Something no antibiotic could kill. Tiny is alive because his doctors resorted to a treatment out of the last century: cutting away his infected flesh.
(More beepers, more hospital personnel)
CARTY: Antibiotics are failing us and people are dying. The US Centers for Disease Control estimates 13,000 Americans die annually because of infections that antibiotics can no longer cure. It's a brave new world, and it frightens Tiny's doctor, Mark Huele.
HUELE: Organisms are arising that are very resistant and they aren't all new and unheard of organisms. A lot of them are old standbys that we thought we had nailed down very effectively. It's a very scary proposition.
CARTY: It's scary because it's challenging the way we think about medicine and the natural world. We used to think that bacteria were a problem and antibiotic drugs were the solution. Now, that equation doesn't work. Because our drugs have changed the natural world, and that change may mean the end of an era in modern medicine. An era that began not so long ago.
(Recording: "Here at St. Mary's Hospital Medical School in Paddington, through this very window, a speck of mold blew in and settled onto Professor Fleming's culture plate." Jazz music plays...)
CARTY: In 1928 Alexander Fleming found some curious green mold growing on a petri dish, and it was killing the bacteria around it. Before Fleming stumbled upon what he called penicillin, bacteria were the world's deadliest scourge. They killed half of all surgery patients, a third of pneumonia cases, almost everyone who got meningitis. In war, more people died of infections than from gun wounds. What a difference a drug makes.
(Recording: dramatic background music: "Disease, whose guerrilla warfare against the Red Cross flag has hitherto out-generalled even the greatest commanders, suffers a setback, thanks to the new miracle drug penicillin...")
LEVY: Penicillin was, of course, the first miracle drug. Why? Because it was so wonderful at killing bacteria and not harming the person. And patients who had terminal illnesses with a bacterial infection were somehow revived.
CARTY: Dr. Stuart Levy is a Professor of Microbiology at Tufts University School of Medicine in Boston. Levy is also one of the leading scholars on antibiotic resistance and the author of The Antibiotic Paradox. He points out that within years of its appearance, some bacteria developed a resistance to penicillin. But no matter. Drug companies just developed new antibiotics.
(Jazz music plays.)
LEVY: Tetracyclines, and chloroenphenicols, and cyclosporins, and the other aminoglycocides like gentomycin. they all came relatively soon in the '50s and '60s. And then discovery was slower. We still had some coming out in the '70s, derivatives of the ones that were found first. Then the 1980s were a little less, and then we get to the '90s with none.
CARTY: Today there are no new antibiotics about to come on the market. Meanwhile, bacteria have made an amazing comeback. For every antibiotic in use, there is at least one resistant bacteria. Some bugs can defeat almost all of them. That leaves us exposed to dozens of diseases, some of them very common, and increasingly dangerous.
LEVY: Start right from the top. Ear infections in kids, which then may be in meningitis, which is severe. The organism which causes strep throat. You get pneumonias which are resistant. Urinary tract infection: how many women have found that they start with one antibiotic, didn't work, I've got to start another one, then I've got to start another one. You have infections following surgery, you have abscesses, blood-borne infection...
CARTY: But how did this happen? How do bacteria become resistant to antibiotics? In a word: evolution. Like all organisms, bacteria evolve in response to changes in their environment, and antibiotics introduce a huge change in a bacteria's environment: a new selective pressure, as evolutionary biologists call it. At first, antibiotics kill all bacteria. But occasionally, some bacteria have little mutations that give them a survival advantage. They defy antibiotics. And since the susceptible ones are killed, the resistant ones can simply multiply freely. Stuart Levy says it's not such an unfamiliar process.
LEVY: It makes me think about the old days, perhaps, when herbicides and pesticides being used on plants were not so specific and if you overused them, you essentially cleared out the lawn. And the only thing left is a single plant of something like crabgrass, or another weed, which is resistant. Well, in that area now, that plant can multiply without any competitors, and what you're left with is a lawn of weeds resistant to the very therapy you used. And I think that that's what happens in a microcosm, in a small way, when you take an antibiotic.
CARTY: And don't underestimate the lowly germ. Since the discovery of penicillin, we humans have evolved a mere 2 generations. But in that same period, bacteria, which reproduce every 20 minutes, have gone through the equivalent of 18 million years of human evolution. They've learned a lot. Like how to pick up resistance from other species of bacteria, even from viruses. So even without the presence of antibiotics, normal bacteria can pick up resistance defenses from resistant bacteria. Dr. Michel Bergeron is the head of infectious disease research at the Laval University Hospital in Quebec City. He likes to use a metaphor to explain bacterial defense systems.
(Dramatic film soundtrack music plays)
BERGERON: Just imagine an army attacking a city. But a walled city. The antibiotic is the army here. The army goes in.
(More dramatic music; thousands of movie extras cry out)
BERGERON: The bacteria will have walls; that's the first line of defense of the bacteria. Some bacteria don't let the army in. The wall of the city becomes much thicker because they've been exposed to these antibiotics.
(Different war music: exploding bombs)
BERGERON: Now, if you're successful, and you breach the wall with your antibiotic or with your army, you go into the city. Now the second line of defense are soldiers within the city.
(Hollywood war continues: a man shouts, "... attack. We need more men out here!"...)
BERGERON: These are enzymes. The bacteria have soldiers that we call enzymes, and they're just things that destroy the army or the other soldiers or the antibiotic.
("Hold your fire...hold your fire. Take out!" Bomb explosions.)
BERGERON: So you see there's many lines of defense.
CARTY: And we are the ones who've made this all possible. By trying to kill bacteria with antibiotics, we have instead given them new life. Dr. Stuart Levy has seen patients die as a result. One was a man he was treating for leukemia and for what seemed like just a minor infection.
LEVY: We had every confidence that we were going to take care of the infection and take care of his leukemia. It was instead the infection that we weren't able to treat. And the infection got ahead too fast. Then I found out that he routinely treated himself, he had a relationship with his physician whereby he could gain access to any antibiotic he wanted. So in a sense, as he told me, he would have a medicine chest loaded with different antibiotics, and sometimes he would call his physician and sometimes he wouldn't. He'd just take them.
CARTY: Antibiotic misuse gives bacteria a perfect environment for developing resistance. And there are many kinds of antibiotic misuse. There's the doctor who over-prescribes antibiotics. There's the patient who demands antibiotics for things like a common cold, which is caused by a virus, not a bacteria. There's the working parent who doesn't complete a full course of antibiotics for a child and who keeps the remnants in the medicine chest to use at the next sign of a cold. Big mistakes. Such usages kill off sensitive bacteria that could keep infections out and allow resistant ones to develop and to come in. And then there's the problem of antibiotics in the food system. Almost half of all antibiotics are used in agriculture to help fatten our cattle and chickens and pigs. People can acquire resistant bacteria at the dinner table. And resistant bacteria are increasingly common, in our bodies and in our environment.
LEVY: In fact antibiotics have put a stress on the environment and on ecology, because the bacteria that we now see out there in the waters, in certain areas, hospitals, sewage systems, they're all resistant. Whereas before, they were consisting mostly of susceptible bacteria.
CARTY: Dr. Levy believes we have altered bacteria more in the past 50 years than in their previous 4 billion years of existence. And it's too early to know what those alterations mean for all the ecosystems where bacteria live.
LEVY: It's hard to make a comparison with other forms of ecologic change, such as burning of the rainforest, but I must say, counting the numbers of types of living organisms affected, then antibiotics are doing a similar effect.
(Clacking sounds in a laboratory)
CARTY: In his laboratory in Quebec City, Dr. Michel Bergeron is trying to find a partial solution for antibiotic resistance. There would be less resistance, he explains, if doctors could use the right antibiotic on the right bug. However, it currently takes 48 hours to get bacterial test results. So when doctors first see a patient, they often prescribe a broad spectrum antibiotic to kill as many possible kinds of bacteria.
BERGERON: Well by doing that, broad spectrum antibiotic favors resistance. Because you expose the microbe, who is very smart, to your best drug. So what does the microbe? He adapts himself. And becomes resistant. My solution is that we have to develop what I call rapid diagnostic tests that will allow the doctor to have the result of the microbe that cause the infection within an hour or so.
CARTY: Dr. Bergeron is developing kits for rapid diagnosis of bacteria. Patents are pending; talks are underway with drug companies. But this is all several years away. Meanwhile, the best medicine may be less medicine. European studies suggest that when antibiotics are limited, bacteria lose their resistance and become susceptible once again. Our antibiotics need not become obsolete, though they will never again be miracle drugs. What doctors fear most is what they call the event. There are bacteria now that are resistant to all antibiotics, but fortunately these bacteria are not very lethal. The fear is that one day, and it's a matter of when, not if, that total resistance will be picked up by a deadly bacteria. The Centers for Disease Control says that event could challenge the entire medical system. Dr. Michel Bergeron agrees.
BERGERON: I think we really were controlling our universe and controlling the bacteria very well up to now. I call it an apocalypse because at this stage we're not ahead. The bacteria is ahead. The bug is ahead of man right now.
(Hospital beeper)
CARTY: For Living on Earth, I'm Bob Carty.
(Music up and under)
CURWOOD: We'll come back to our reports on antibiotic resistance in just a moment. But first, let us know about your environmental health concerns. Please give us a call at 1-800-218-9988. That's 1-800-218-9988. Or you can write to us at Living on Earth, Box 639, Cambridge, Massachusetts 02238. That's Living on Earth, Box 639, Cambridge, Massachusetts 02238. Our Internet address is LOE@NPR.ORG. That's LOE@NPR.ORG. Transcripts and tapes are $10.
Evolutionary Medicine: Rethinking the Origins of Disease
CURWOOD: And just what can we do about this growing resistance of germs to antibiotics? There's a man in the San Francisco area who's been doing a lot of thinking about this, and he's come up with some answers. His name is Marc Lappé, and he's a research pathologist. His new book is called Evolutionary Medicine: Rethinking the Origins of Disease. Dr. Lappé says we have to remember evolution and that humans and bacteria evolve together. And that since bacteria can have a new generation every 20 minutes and adapt to environmental changes a lot faster than we humans can, we humans have to be smarter and work with the balance of nature instead of against it.
LAPPÉ: Not only do we have an intimate relationship with the bacteria that live in and on us, but we're in a very tight ecological relationship with virtually all the other bacteria in the world. But this image that we're facing an inimical horde of bacteria in part has led to the attempt not only to isolate ourselves from it, but with the mistaken belief that we can actually annihilate bacteria with antibiotics or other controls.
CURWOOD: In the evolutionary model of disease, what are the conditions that favor the appearance of new ailments?
LAPPÉ: We've essentially created our own nightmare by neglecting the value of vaccines, immunization, and natural controls and instead have relied entirely on this myth that a chemotherapeutic approach is an impenetrable barrier. We also share ecological niches wherever we live with the bacteria and viruses around us. When we disturb those niches, by taking enormous amounts of antibiotics, our bodies respond by allowing new organisms to overgrow our natural organisms. That's the origin of the epidemic of yeast infections in women, for instance. But on a grander scheme in the natural environment, for instance when we use antibiotics in feed lots, we cause an epidemic of resistance to the very antibiotics that we intend to use for treating disease later in humans.
CURWOOD: So by changing the earth's ecology, we increase the likelihood of us getting diseases; is that what you're saying?
LAPPÉ: At this moment we are controlling the evolution, not just by decimating species and annihilating swaths of rain forest, but by shifting the balance towards organisms that can thrive in the environment that we create.
CURWOOD: Can you tell us how evolution has led to diseases in some ancient societies that we might know about?
LAPPÉ: We think for instance that the malarial parasite emerged when we started to practice agriculture in central Africa, and we pushed into environments that were inhabited by lowland gorillas or chimps that carried a rather benign form of the plasmodium parasite. By creating new environments we also encourage the outgrowth of the anopheles mosquito and we thereby created the havoc that was then wreaked on populations in Africa by our own doings. But in many of those societies, most diseases were limited by the structure and nature of the social arrangements that people had. When we concentrated into towns, cities, and ultimately ghettos, we think we created the conditions for the explosive outburst of disease.
CURWOOD: How has the change in our social conditions pushed the evolution of disease?
LAPPÉ: One example would be the explosion of Lyme Disease, which now has been reported in every state in the Union. This is a condition that's brought about by moving human populations too close to natural populations that are the natural vectors or carriers of this disease. We've allowed the explosion of the deer population by eliminating predators and permitting the regrowth of forests. We put humans in these lovely suburban environments only to find that as they and their dogs walk thorough paths through the woods or adjacent to wild areas, they're picking up ticks that carry the beryllia organism that causes Lyme disease. This has been a dramatic change in the ecology, and it's been accompanied by the dramatic emergence of a new disease.
CURWOOD: So how do we fix this?
LAPPÉ: My idea is to use evolutionary strategies. We know what the intermediate hosts are. We know, as we did with rabies vaccine, that we can feed the wild population vaccines which will be active when ingested. These vaccines can be directed not against the beryllia organism but against the tick.
CURWOOD: With all the antibiotic resistance that's showing up in hospitals, medical professionals - you know, they're saying we're in trouble. But do you think they're really ready to change?
LAPPÉ: They're not ready to change; they have not learned the lesson that more is not better. That certain antibiotics should be absolutely kept in a locked safe, which is done in Sweden and Norway, where they're kept in reserve for emergencies. These are valuable commodities that are being squandered.
CURWOOD: What can individuals do?
LAPPÉ: First of all they can keep from annihilating their immune systems. Don't go out and sunbathe, for instance. Good nutrition, rest, are the key elements for maintaining the immune system. Be sure that you have an adequate intake of key vitamins that are essential for the function of the immune system, like vitamin C. Vitamin A is an immune stimulant; vitamin E is an important anti-oxidant. Stay off meth-amphetamines and things that run the system dry, and avoid medical products and devices like silicone-containing devices that screw up the immune system. Because chronic inflammation may activate the immune system in totally non-evolutionarily adaptive ways.
CURWOOD: I want to thank you for taking this time with us.
LAPPÉ: You're very welcome.
CURWOOD: Marc Lappé is a research pathologist and author of Evolutionary Medicine: Rethinking the Origins of Disease.
(Music up and under)
CURWOOD: Living on Earth comes to you with help from Peter Thomson, Deborah Stavro, Kim Motylewski, George Homsy, Constantine Von Hoffman, Jan Nunley, and Julia Madeson. Thanks, too, to Jessika Bella Mura, Heather Corson, David Dunlap, Alex Garcia-Rangel, and Christopher Rose. And a special thanks to Jim Donahue. Our WBUR engineers are Louie Cronin and Mark Navin. Our theme music was composed by Michael Aharon.
Living on Earth is a project of the World Media Foundation, and recorded at WBUR, Boston. I'm Steve Curwood, executive producer. I'll be back next week; be sure to tune in.
ANNOUNCER: Living on Earth is made possible with major support from the Geraldine R. Dodge Foundation; the Joyce Foundation; the National Science Foundation for coverage of science and the environment; and all-natural Stonyfield Farm Yogurt - whether supporting worthwhile causes or producing healthy foods, Stonyfield's goal is to make you feel good inside.
NPR ANNOUNCER: This is NPR, National Public Radio.
This Week's Books
Living on Earth wants to hear from you!
Living on Earth
62 Calef Highway, Suite 212
Lee, NH 03861
Telephone: 617-287-4121
E-mail: comments@loe.org
Newsletter [Click here]
Donate to Living on Earth!
Living on Earth is an independent media program and relies entirely on contributions from listeners and institutions supporting public service. Please donate now to preserve an independent environmental voice.
NewsletterLiving on Earth offers a weekly delivery of the show's rundown to your mailbox. Sign up for our newsletter today!
 Sailors For The Sea: Be the change you want to sea.
Sailors For The Sea: Be the change you want to sea.
 The Grantham Foundation for the Protection of the Environment: Committed to protecting and improving the health of the global environment.
The Grantham Foundation for the Protection of the Environment: Committed to protecting and improving the health of the global environment.
 Contribute to Living on Earth and receive, as our gift to you, an archival print of one of Mark Seth Lender's extraordinary wildlife photographs. Follow the link to see Mark's current collection of photographs.
Contribute to Living on Earth and receive, as our gift to you, an archival print of one of Mark Seth Lender's extraordinary wildlife photographs. Follow the link to see Mark's current collection of photographs.
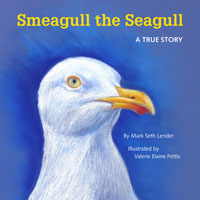 Buy a signed copy of Mark Seth Lender's book Smeagull the Seagull & support Living on Earth
Buy a signed copy of Mark Seth Lender's book Smeagull the Seagull & support Living on Earth

